Renal Tubular Acidosis (RTA) might sound complex, but it’s a condition that affects the body’s ability to maintain a proper acid-base balance. Your kidneys play a critical role in filtering blood, removing waste, and balancing various substances, including acids and bases. When this system falters, conditions like RTA can emerge. This blog delves into the nuances of RTA, its types, symptoms, causes, complications, treatments, and how to navigate life with this condition.


What is Renal Tubular Acidosis (RTA)?
Renal Tubular Acidosis (RTA) refers to a group of disorders in which the kidneys fail to properly acidify the urine. This disrupts the body’s acid-base equilibrium, causing an accumulation of acid in the blood, a condition known as acidosis. Unlike kidney failure, RTA occurs despite the kidneys’ overall filtering capacity being relatively intact.
Types of Renal Tubular Acidosis
RTA is classified into four major types based on the underlying defect:
Type 1 (Distal RTA):
The kidneys are unable to excrete hydrogen ions (acid) into the urine, leading to acidic blood and alkaline urine.
Type 2 (Proximal RTA):
Here, the kidney fails to reabsorb bicarbonate effectively in the proximal tubules, leading to bicarbonate loss in the urine.
Type 3 (Mixed RTA):
A rare combination of Type 1 and Type 2 RTA characteristics.
Type 4 (Hyperkalemic RTA):
This type is linked to reduced aldosterone levels or kidney insensitivity to aldosterone, causing high potassium levels in the blood and metabolic acidosis.
Each type of RTA has distinct causes and treatment approaches.
Exercises for Heart Health
The symptoms of RTA vary depending on the type and severity but may include:
Fatigue and muscle weakness
Poor growth in children (growth retardation)
Nausea and vomiting
Increased urination and thirst (polyuria and polydipsia)
Kidney stones or nephrocalcinosis
Bone pain or fractures (due to loss of calcium from bones)
If left untreated, RTA can have long-term consequences on kidney health and overall well-being.
Causes of Renal Tubular Acidosis
RTA can be caused by various factors, including:
Genetic predisposition: Inherited conditions such as autosomal dominant or recessive disorders.
Autoimmune diseases: Conditions like Sjögren’s syndrome or lupus.
Medications: Certain drugs, including amphotericin B or non-steroidal anti-inflammatory drugs (NSAIDs).
Metabolic disorders: Hypercalcemia (high calcium levels), hypokalemia (low potassium levels).
Other kidney conditions: Chronic kidney disease, obstructive uropathy.
Understanding the underlying cause is essential for tailoring effective treatment strategies
Complications of Renal Tubular Acidosis
Untreated RTA can lead to several complications:
Kidney Stones and Nephrocalcinosis:
Due to calcium deposits in the kidneys, leading to reduced kidney function over time.
Bone Weakening:
Acidosis may cause calcium leaching from bones, increasing the risk of fractures.
Growth Problems in Children:
Prolonged acidosis can delay growth and development in pediatric cases.
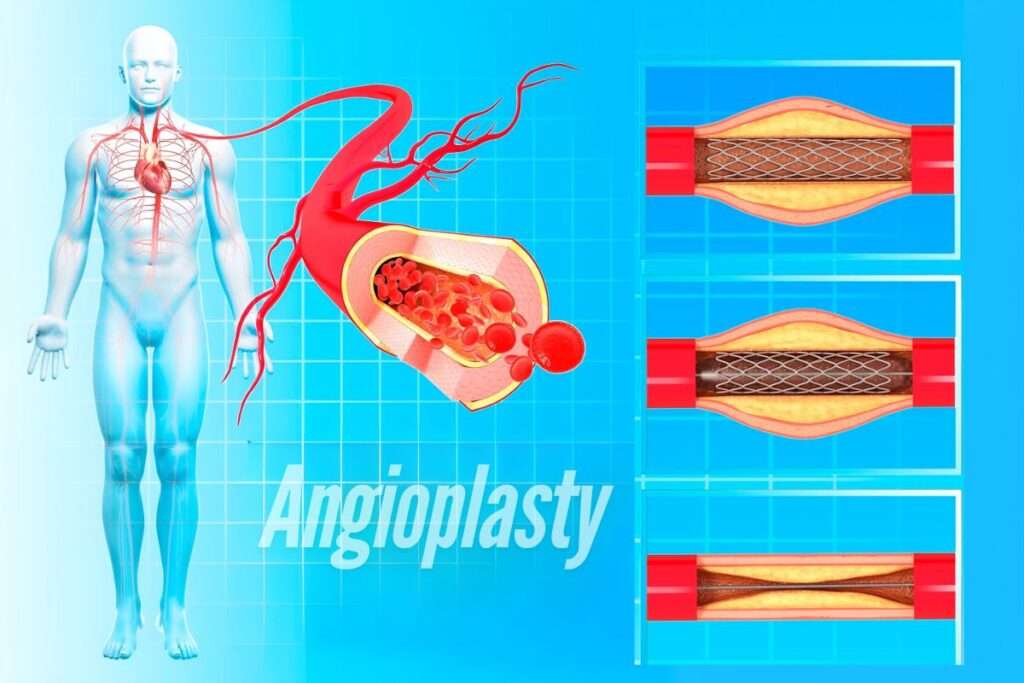
Electrolyte Imbalance:
Issues like low potassium (hypokalemia) or high potassium (hyperkalemia in Type 4 RTA) can impact heart and muscle functions.
Early diagnosis and management are crucial to prevent these complications
Treatment for Renal Tubular Acidosis
The primary goal of RTA treatment is to correct acidosis and maintain a balanced pH. Treatments include:
Alkali Replacement Therapy:
Sodium bicarbonate or potassium citrate is commonly used to neutralize acid levels.Potassium Supplements:
For hypokalemia, potassium supplements may be necessary.
Dietary Adjustments:
A low-sodium, balanced diet can help manage symptoms and prevent complications.
Treating Underlying Conditions:
Addressing the root cause, such as autoimmune diseases or genetic factors, is equally important.
Regular monitoring of blood and urine parameters ensures effective management and minimizes risks.
Frequently Asked Questions
RTA is relatively rare. While it can occur in individuals of any age, certain types, such as Type 2 RTA, are more commonly seen in children, while Type 4 RTA is often associated with adults with diabetes or chronic kidney conditions.
Diagnosis typically involves:
- Blood tests to measure pH, bicarbonate, and potassium levels.
- Urine tests to check acid excretion and pH levels.
- Imaging studies, such as ultrasounds, to identify kidney stones or structural abnormalities.
A thorough medical history and physical examination are also essential.
RTA can affect various bodily systems:
- Skeletal system: Bone demineralization leading to pain or fractures.
- Growth and development: In children, prolonged acidosis can impair normal growth.
- Muscle function: Electrolyte imbalances can weaken muscles and cause fatigue.
Early signs include unexplained fatigue, persistent muscle weakness, or recurring kidney stones. A detailed medical evaluation is necessary to confirm the diagnosis.
Managing RTA involves lifestyle adjustments and regular medical care:
Medication adherence: Regularly take prescribed alkalinizing agents.
Diet: A diet low in salt and rich in fruits and vegetables supports acid-base balance.
Hydration: Stay well-hydrated to prevent kidney stones.
Follow-ups: Regular check-ups with your doctor to monitor progress and prevent complications
Living with Renal Tubular Acidosis
Although RTA requires lifelong management, the outlook is positive with proper treatment. By adopting healthy lifestyle habits, maintaining regular medical follow-ups, and staying informed, individuals with RTA can lead fulfilling lives. Remember, early detection and intervention are key to preventing complications and ensuring a good quality of life.
If you or someone you know experiences symptoms of RTA, consult a healthcare professional at Archana Hospital. Our specialists are equipped to provide accurate diagnosis, personalized treatment plans, and compassionate care.