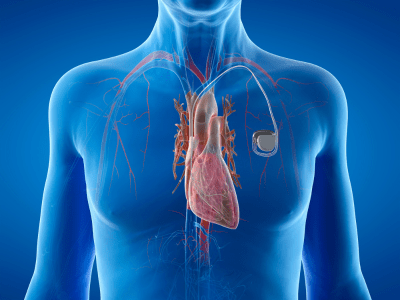
What is a Pacemaker?
A Pacemaker is a small device implanted under the skin to regulate heart rhythm by sending electrical pulses to the heart muscle, ensuring it beats regularly and efficiently. It’s used to treat arrhythmias and improve overall heart function.
The main function of a pacemaker is to monitor the heart’s electrical activity and intervene when it detects irregularities. The heart relies on electrical impulses to contract and pump blood effectively. In some individuals, these impulses may become irregular or too slow, leading to symptoms such as dizziness, fainting, shortness of breath, or fatigue. A pacemaker helps by sending electrical impulses to the heart muscle, ensuring it beats at a regular rhythm and maintains an adequate heart rate.