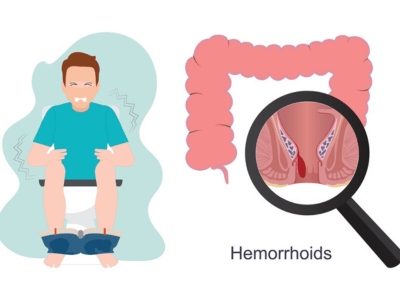
Hemorrhoidectomy
The surgical treatment used to eliminate hemorrhoids is called a hemorrhoidectomy. Hemorrhoids usually don’t require surgery, but if they persist or create significant problems, a hemorrhoidectomy can permanently remove them. The process is straightforward, although recuperation could be a little challenging. Take our recommendations to reduce discomfort and avoid constipation.

What is a Hemorrhoidectomy?
The surgical treatment used to eliminate Hemorrhoids is called a hemorrhoidectomy. Enlarged blood vessels in the anus (butthole), known as hemorrhoids can occasionally result in painful symptoms, including bleeding and anal pain.
Hemorrhoids are pretty frequent and often not harmful. Most won’t even need surgery or other medical care. However, a hemorrhoidectomy may be the best course of action for some hemorrhoids and in some situations.
Risks / Benefits
What benefits does hemorrhoidectomy offer in comparison to other hemorrhoid treatments?
The main benefit is that it functions. Surgically excised hemorrhoids usually don’t recur. Surgery should ultimately provide permanent relief, even though the recovery period is longer than other treatments.
Another crucial option in an emergency is a hemorrhoidectomy. Surgery can be used to treat a thrombosed or strangulated hemorrhoid quickly and avoid worsening the condition.
What makes a Person get a Hemorrhoidectomy?
If your hemorrhoids are more complicated than usual, your doctor may suggest hemorrhoidectomy surgery. The following complications could necessitate a hemorrhoidectomy:
Prolapse: This indicates that your hemorrhoids have descended from inside your anus and are now protruding from the orifice, increasing the risk of irritation, bleeding, or injury. Prolapse is a progressive condition that often gets worse with time. Initially, Grade II hemorrhoids may only momentarily protrude from your anus during a bowel movement. However, your provider could advise removing them if you have to put them back in (Grade III) manually or if they won’t go back in at all (Grade IV).
Thrombosis: This is the point at which hemorrhoid has swelled to the point where blood clots inside it, stopping blood flow. The color of thrombosed hemorrhoids is purple-blue. They may cause excruciating agony. They may occasionally burst, heavily bleeding. It will eventually heal on its own if you do not seek treatment immediately. But you might prefer surgery during the excruciating first 72 hours.
Constriction: Incarcerated hemorrhoids are another name for Grade IV hemorrhoids that have prolapsed and refused to retract. A hemorrhoid in prison runs the risk of strangling itself. When something is strangled, it indicates that its circulation has been cut off and it is stuck in a constricted area. There is an urgent situation. In contrast to thrombosis, strangulation is not a self-limiting illness—gangrene results from the strangulated tissues’ eventual death.
Return: Hemorrhoids can recur after less intrusive treatments or don’t go away. This may have a significant long-term effect on your quality of life. Hemorrhoidectomy has a 95% success rate when other therapies are unsuccessful. You may decide to get a hemorrhoidectomy to permanently remove these hemorrhoids, even if you don’t have any other difficulties.
What can I anticipate from my hemorrhoidectomy recovery?
Following a hemorrhoidectomy, you could anticipate varying degrees of:
Bleeding: Following a hemorrhoidectomy, some bleeding is typical, particularly after a bowel movement (poop). There may be blood on your toilet paper or in your feces. Along with some clear or yellow discharge, you can also notice some in your underpants. To assist in absorbing the liquid, you can use gauze or a sanitary pad. This may go on for a month or longer. There shouldn’t be much blood. If you strain too hard to void, you run the risk of splitting the wound open, which could lead to more serious bleeding. To avoid this, constipation must be avoided. Occasionally, some patients have acute bleeding following surgery.
Swelling: Following a hemorrhoidectomy, swelling is typical. Anus swelling might have a feeling akin to hemorrhoids. It’s possible that you still think of them or that they’ve returned, but these are false impressions. Occasionally, a skin tag or lump may appear where the wound was made, which can also be misleading. Usually, these disappear after you’ve healed. Everyone’s healing process is different. Applying ice wrapped in a towel to the incision a few times a day for ten minutes will help minimize swelling. Lying on your stomach with a pillow under your hips can also be beneficial. Try to sleep in this manner.
Pain: After a hemorrhoidectomy, some pain is to be expected, and most patients report relatively high pain levels. However, you ought to be able to use medicine to control your pain. Typically, medical professionals provide a range of pain management techniques, such as topical and oral drugs and gentle wound care. Start taking your medications as soon as you feel any discomfort following your procedure to avoid it altogether. Most report that, after two weeks, the pain has subsided. Consult your healthcare practitioner if your discomfort persists for more than two weeks, if you find it difficult to manage, or if it keeps you from urinating or passing gas.
Recovery after Haemorrhoid Removal
Following your Hemorrhoid removal, you may be advised to do the following self-care measures:
Medication: Take your prescriptions exactly as directed by your physician. This could involve laxatives, antibiotics, and painkillers.
Activities: Make sure you get enough sleep and time to be active. Walking is a wise decision.
Diet: Your doctor may advise you on a diet that reduces the likelihood of constipation.
Additional actions could be using ice packs, taking stool softeners, taking a sitz bath, and drinking plenty of water.
What are the possible risks or complications of hemorrhoidectomy surgery?
Among the short-term hazards of surgery are:
Thrombi.
Negative effects of the anesthetic.
Infection of the wound.
Excessive loss of blood.
Among the issues that could arise when you’re recovering are:
Possible long-term complications that can develop include:
Gradual recovery.
Severe pain even after taking medicine.
Urinary retention due to pain when peeing.
Constipation due to pain when pooping.
Narrowing of your anal canal from excessive scarring (anal stenosis).
Difficulty holding in your bowel movements due to muscle or nerve damage (fecal incontinence).
With careful technique, serious complications are rare.
Who is not a candidate for a hemorrhoidectomy?
Suppose you have specific medical conditions that could raise your risk of significant complications from the treatment. In that case, your healthcare professional might not propose hemorrhoidectomy for you. Among them are:
Immunosuppression.
Inflammatory bowel disease (IBD).
Bleeding disorders.
Portal hypertension.