H3N2 Virus and Preventing Its Spread
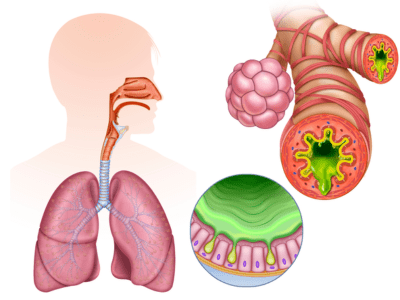
The H3N2 virus is a subtype of the influenza A virus that can cause respiratory illness in humans. Symptoms of H3N2 virus infection are similar to those of other types of influenza, including fever, cough, sore throat, runny or stuffy nose, muscle aches, and fatigue. In severe cases, it can lead to complications such as pneumonia, bronchitis, or even death, especially in the elderly, young children, and people with weakened immune systems.
The H3N2 virus is highly contagious and can spread from person to person through the air when an infected person coughs or sneezes or by touching contaminated surfaces and then touching one’s nose, mouth, or eyes. Therefore, taking steps to prevent its spread is essential to avoid getting sick and reduce the risk of outbreaks.
Preventing the Spread of H3N2 Virus :
Get vaccinated: An annual flu vaccine is the best way to protect yourself from getting infected with the H3N2 virus or other influenza strains. The vaccine is recommended for everyone over the age of six months, especially those at high risk of complications from the flu, such as pregnant women, older adults, and people with chronic health conditions.
Practice good hygiene: Wash your hands frequently with soap and water or use an alcohol-based hand sanitizer, especially before eating or touching your face. Cover your mouth and nose with a tissue or your sleeve when coughing or sneezing, and dispose of used tissues immediately.
Cover Your Mouth and Nose: Cover your mouth and nose with a tissue or sleeve when coughing or sneezing. Dispose of used tissues immediately.
Avoid close contact with sick people: If you are sick, stay home to avoid spreading the virus to others. If you are healthy, try to stay away from people who are sick, especially if they have flu-like symptoms.
Clean and disinfect frequently touched surfaces: Use a disinfectant cleaner to wipe down commonly touched surfaces, such as doorknobs, light switches, keyboards, and phones, to reduce the spread of germs.
Practice good health habits: Take care of your overall health by getting enough sleep, eating a balanced diet, exercising regularly, and managing stress. A healthy lifestyle can boost your immune system and reduce the risk of getting sick.
Therefore reduce the risk of getting infected by getting vaccinated and adopting other hygiene practices. Do not hesitate to call a Specialist at Archana Hospitals if you have further questions.